Interdisciplinary team leads push for revision of guidelines for evaluation of use, optimization of biologic therapies
 During his college wrestling career, Michael Baria, MD, assistant professor of Physical Medicine and Rehabilitation at The Ohio State University College of Medicine, underwent four knee surgeries. Diligent care from his medical team enabled him to get back to the mat.
During his college wrestling career, Michael Baria, MD, assistant professor of Physical Medicine and Rehabilitation at The Ohio State University College of Medicine, underwent four knee surgeries. Diligent care from his medical team enabled him to get back to the mat.
Today, as a physician specializing in sports medicine, Dr. Baria is able to flex different muscles to help patients overcome conditions of the musculoskeletal system and heal quicker from orthopedic injuries. He employs cutting-edge therapy, called orthobiologic injection-based therapy, to treat damaged and injured joints. Alongside his interdisciplinary team, he also works to ensure medical advancements are made employing the appropriate processes.
“Orthobiologics are a group of minimally invasive treatment options that use biological substances found naturally in the body that may hasten healing,” says Dr. Baria.
These substances are human cells, which range from platelets to bone marrow to adipose, connective tissue composed of fat cells. They can easily be extracted from a patient and injected into the site of damage. Platelet-rich plasma (PRP) is anti-inflammatory and helps promote tissue healing and is mostly used to treat arthritis, tendinitis and athletic injuries. Another common procedure is called bone marrow aspirate concentrate. This procedure involves taking bone marrow, concentrating the cells in the office, and then injecting them into a joint, tendon or ligament tear.
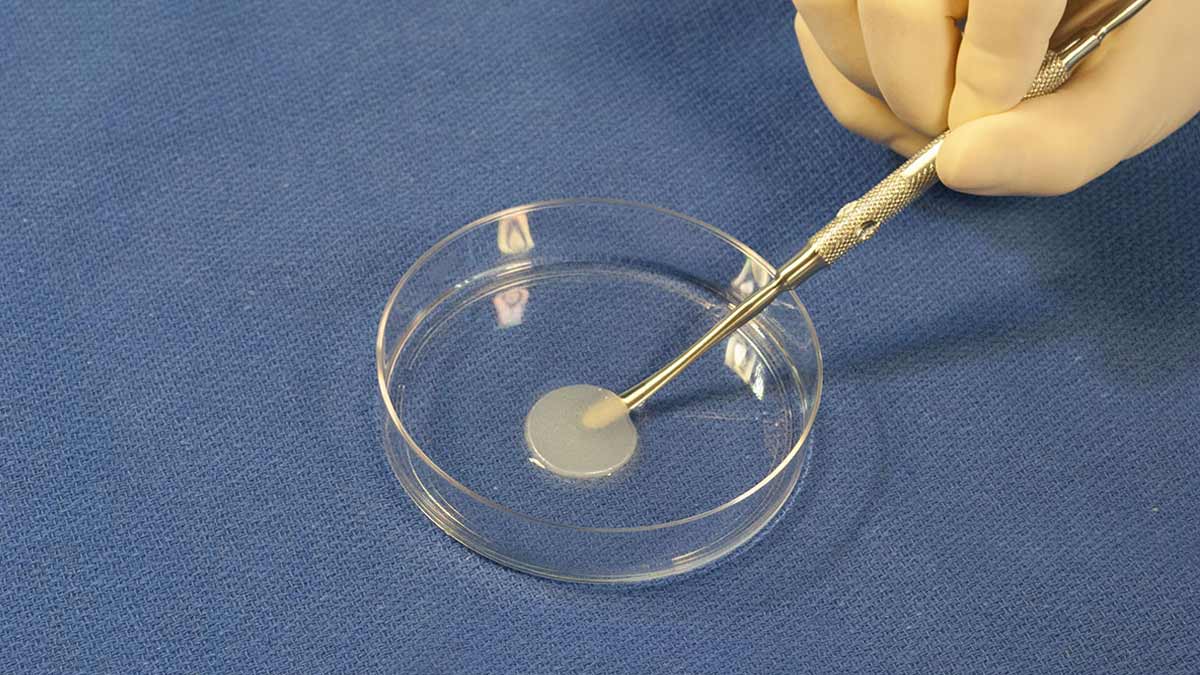 Adipose is also being used as it contains several cell types that have the potential to heal tissue. This newer procedure is easily tolerated, and Dr. Baria recently completed a randomized study examining the effects of adipose on arthritic knees.
Adipose is also being used as it contains several cell types that have the potential to heal tissue. This newer procedure is easily tolerated, and Dr. Baria recently completed a randomized study examining the effects of adipose on arthritic knees.
Since, the use of orthobiologics is on the rise and those working in the field have developed a better understanding of what they need to study further to make additional advancements, Dr. Baria and his team decided it was an ideal time to give the Minimum Information for Studies Evaluating Biologics in Orthopaedics (MIBO) guidelines a deep inspection. The guidelines — developed to provide a consensus framework for improving and accelerating clinical evaluation concerning the use and optimization of these biologic therapies — point toward a better understanding, but in their current form, don’t capture all of the necessary information and are very difficult for researchers to implement.
Dr. Baria and his team’s detailed findings, including how practioners are limited by inadequate reporting of scientific details critical to patient outcomes, was recently published in American Journal of Physical Medicine & Rehabilitation.
In “Is it time to revisit the Minimum Information for Studies Evaluating Biologics in Orthopaedics (MIBO) Guidelines: Platelet-Rich Plasma and Mesenchymal Stem Cells,” Dr. Baria and co-authors W. Kelton Vasileff, MD, David Flanigan, MD, and Sushmitha Durgam, PhD, BVsC, explain how the understanding and terminology for various interventions have rapidly changed and reporting requirements should therefore reflect these changes. They lay out the rationale for why the guidelines should be evaluated and amended depending on the specific orthobiologic under investigation.
Specific to PRP studies, the only major additional requirements are complete blood counts on the whole blood and PRP, which can be performed either in a clinical laboratory or with an in-house cell counter. Dr. Baria says these fairly simple requirements are accessible and not cost prohibitive.
“However, the requirements for mesenchymal stem cells (MSCs) that can self-renew by dividing and can differentiate into multiple tissues including bone, cartilage, muscle and fat cells, and connective tissue warrant further consideration before these become mandatory reporting for orthobiologic studies,” says Dr. Baria.
Dr. Baria argues that MIBO requirements for MSCs are more readily applied to studies that isolate and perform culture-expansion on cells. The criteria in its current form can’t be applied to all clinical studies using interventions like bone marrow concentrate (BMC) or adipose. He adds that few orthopedic centers would be able to contribute to the literature if this is the requirement.
“This could limit the amount of sound clinical data published and available to advance orthobiologics,” says Dr. Baria. “We propose reconsideration and a possible revision of the MIBO guidelines that allow for distinction of MSC studies from interventions like BMC and lipoaspirate and flexibility on reporting.”
Dr. Baria and his team’s dedication to ongoing research enables them to provide evidence-based interventions and pioneer ideas, knowledge and techniques that push discovery in regenerative medicine forward. It also allows them to understand different variables that influence when their patients can safely return to their activities.



