Ohio State researchers isolate biomarker to test for chronic fatigue syndrome
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and Gulf War illness are complex, chronic diseases with overlapping symptoms and no definitive way to diagnose or differentiate between them.
The one symptom they share in common is long-term, disabling fatigue. But widely varying symptoms affecting the immune, endocrine and neurological systems may occur, including muscle and joint pain, concentration and memory problems, headaches, sleep problems, fever, sore throat and tender lymph nodes—symptoms that are common to a number of different illnesses, making diagnosis of ME/CFS even more challenging.
Around 50% of patients who develop ME/CFS report that their symptoms occurred after exhibiting “flu-like” symptoms, leading some researchers to look into the role that certain viruses play in triggering an ME/CFS infection and its impact on the body’s immune system. Viruses such as Epstein-Barr virus, human herpesvirus 6 and varicella-zoster virus, all of which establish latent (persistent) infections in their host, can be periodically reactivated over a person’s lifetime.
Researchers led by cancer biology and genetics professors Marshall Williams, PhD, and Maria Ariza, PhD, at The Ohio State University College of Medicine have looked at the association between these viruses and ME/CFS. They have identified the protein deoxyuridine triphosphate nucleotidohydrolase (dUTPase) as a key modulator of the immune response that contributes to the immunological and neurological abnormalities in some individuals. Their work suggests that the dUTPase protein can be used as a biomarker to identify evidence of the disease observed in a subset of patients, paving the way for early detection and prevention of ME/CFS and related illnesses.
“The impact value of our findings is enormous, when you think about the fact that there is currently no commercially available test to measure the concentration of antibodies against the herpesviruses dUTPase proteins present in patients’ sera,” says Dr. Ariza.
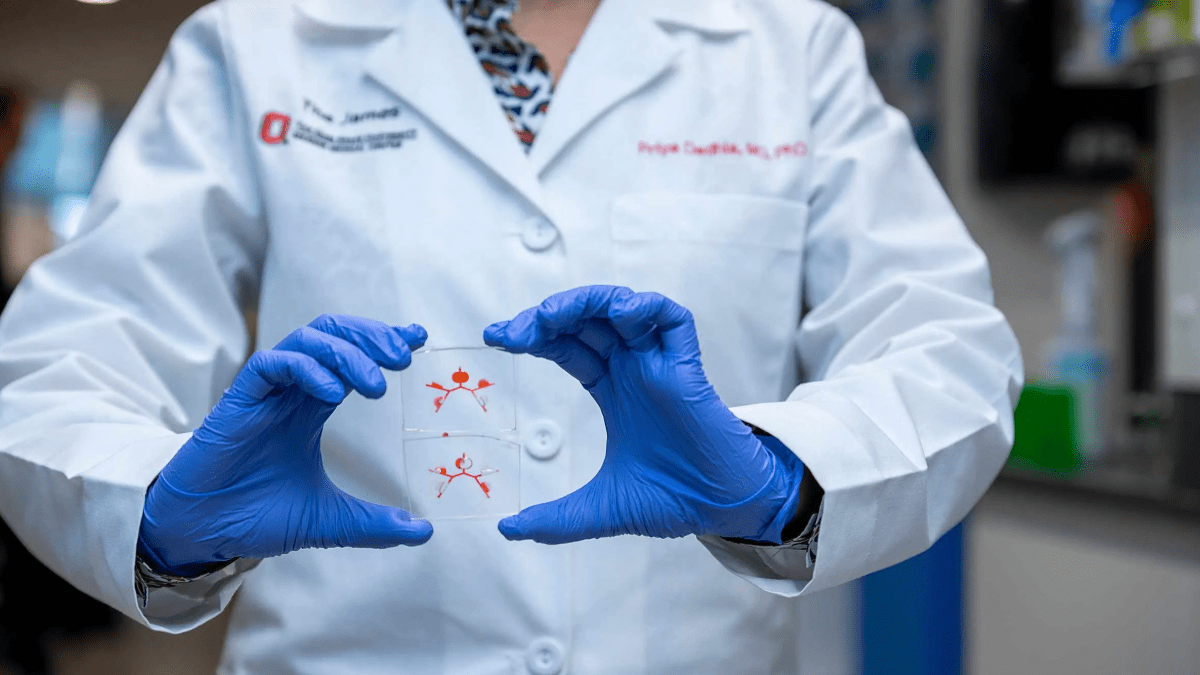
The team is also in the process of developing a single array ELISA test that will allow for the simultaneous quantitation of six different dUTPases, a major milestone that would allow for high throughput screening of a large number of serum samples and aid in diagnosing and, potentially, stratifying patient symptom severity.
“These are very exciting times in our labs, as we currently have NIH funding to validate the dUTPase array ELISA in 4,000 clinical serum from ME/CFS patient cohorts of different severities,” says. Dr. Ariza. “Because it is a noninvasive method, if validated, it could be easily implemented in clinical settings for standard testing.”
Drs. Williams and Ariza are members of an interdisciplinary team of research scientists and clinicians bought together from across The Ohio State University’s vast system of clinical science departments and centers to conduct cutting-edge research in the College of Medicine’s Institute for Behavioral Medicine Research, making up one of the largest contingents of psychoneuroimmunology researchers in the world. Their innovative, high-impact work results from collaborations in areas that include medicine, microbial pathogenesis, nursing, biostatistics, human sciences, microbial infection and immunity, neuroscience, neurological surgery, obstetrics and gynecology, pediatrics, psychiatry and behavioral health, and psychology.