New Gene Therapy Institute positions Ohio State as a leader in translational science
 Each year, two clinical fellows arrive at The Ohio State University College of Medicine and The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute to hone their skills in removing some of the rarest and most dangerous head and neck tumors. They come to learn from a pair of renowned surgeons who pioneered minimally invasive surgical techniques to remove skull base tumors.
Each year, two clinical fellows arrive at The Ohio State University College of Medicine and The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute to hone their skills in removing some of the rarest and most dangerous head and neck tumors. They come to learn from a pair of renowned surgeons who pioneered minimally invasive surgical techniques to remove skull base tumors.
According to the National Cancer Institute, head and neck cancers account for 4% of all cancers in the body. The skull base, a high real estate area of the body where the brain, nerves, vessels and major sensory organs all intersect, is involved in about 0.01% of cancers. It’s a high-risk area with little to no margin for error.
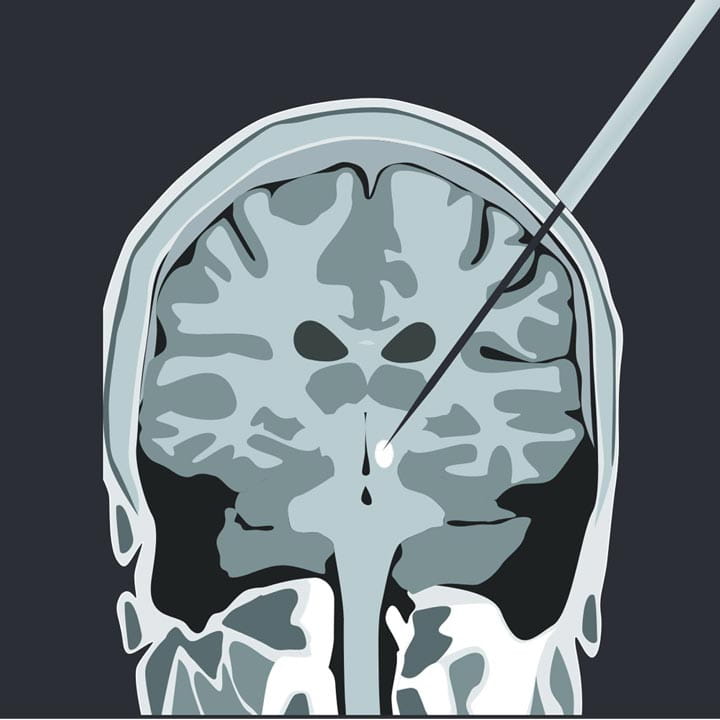
Ricardo Carrau, MD, professor of Otolaryngology – Head and Neck Surgery at the Ohio State College of Medicine, was one of the first surgeons in the world to use an endoscope to enter the nasal cavity and create a surgical path to remove skull base tumors.
His longtime surgical partner, Daniel Prevedello, MD, professor of Neurological Surgery at the Ohio State College of Medicine, removes the tumor if it’s intracranial. They collaborate surgically if the tumor has invaded other areas. The pair then closes together, rebuilding the skull base and nasal passageway.
Dr. Prevedello is one of only a few neurosurgeons in the world who have performed more than 1,000 endoscopic endonasal approach surgeries. Dr. Carrau has completed an estimated 2,000 endoscopic endonasal approach surgeries.
Their combined experience is highly sought after at Ohio State’s Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute. Patients come from all over the world to seek treatment. Therefore, Ohio State Fellows obtain experience with some of the most challenging skull base tumor cases in the world.
“Our idea is to train the next generation,” Dr. Carrau says. “To acquire the experience and to have the volume necessary to continue evolving as a surgeon is unique.”
Both Drs. Carrau and Prevedello host a clinical fellow each year to impart their surgical craft. Clinical fellowships, now in place at Ohio State for 11 years, typically last one to two years depending on the fellow’s previous training.
“When fellows leave Ohio State, they’re able to independently complete their portion of the surgery,” Dr. Prevedello says. “Many go on to work at academic hospitals and some even find their way back to Ohio State.”
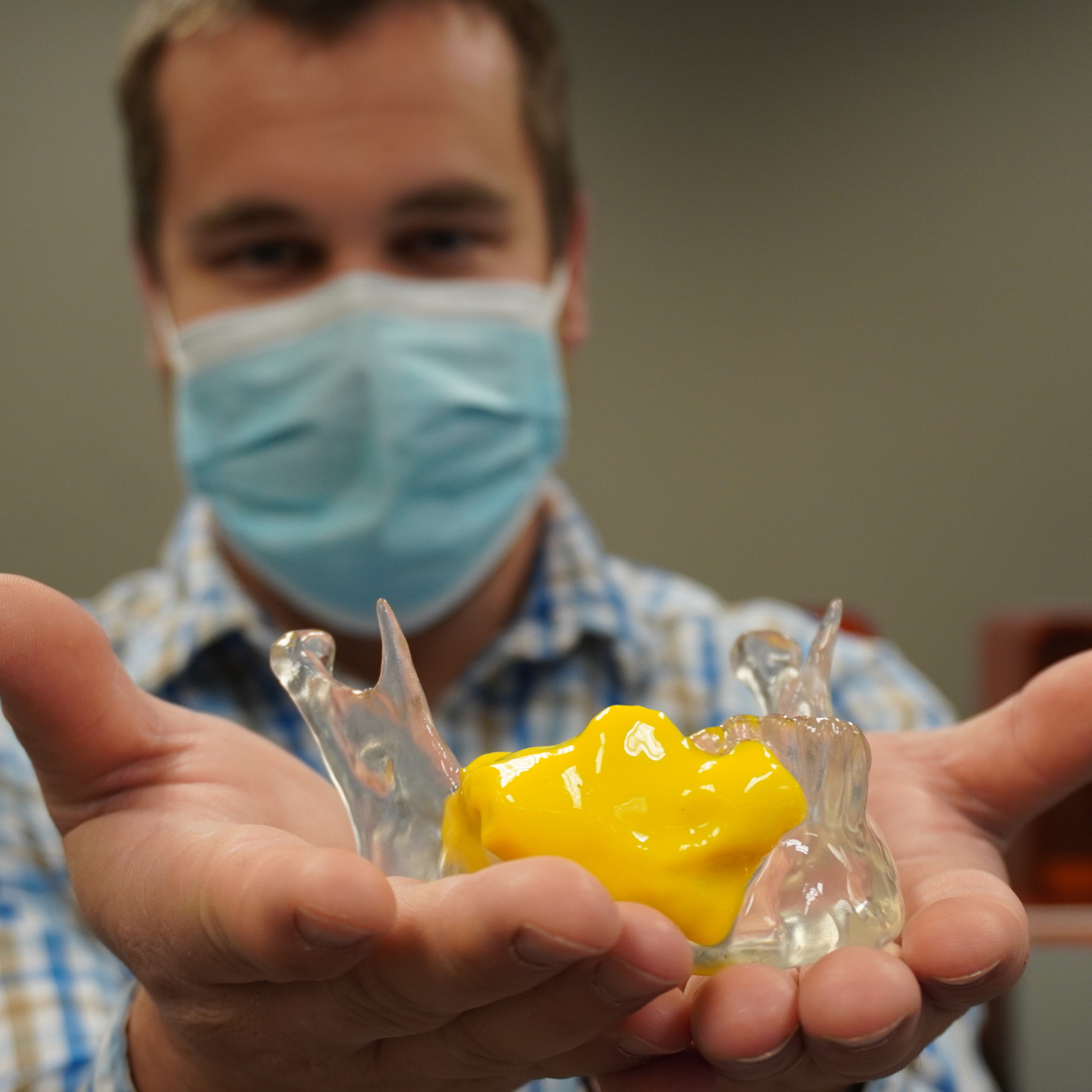
Kyle VanKoevering, MD, assistant professor of Otolaryngology at the Ohio State College of Medicine, was an otolaryngology clinical fellow in the program and was later hired to be part of the skull base surgical team at the OSUCCC – James. He now runs the skull base fellowship program for the Department of Otolaryngology – Head and Neck Surgery. Dr. VanKoevering, who previously studied engineering, also directs Ohio State’s Medical, Modeling, Materials and Manufacturing (M4) Lab to create realistic 3D printed surgical models for surgeons to sharpen their skills before performing complicated tumor surgeries and to plan the reconstruction.
Another former fellow, Douglas Hardesty, MD, associate professor of Neurological Surgery at the College of Medicine, was recruited back to Ohio State to expand the program on the neurological side and serve as co-director of the Anatomy Laboratory Toward Visuospatial Innovation in Otolaryngology and Neurosurgery, a research and education lab.
“It is only through mentorship and fellowship that we can properly teach these techniques to our fellows,” Dr, Prevedello says. “They are our legacy, and they will properly take care of the patients in other parts of the world and in the future.”